Insulin resistance detectable 20 years before diabetes 2 onset
What is Resistance? Insulin and Chronic Disease
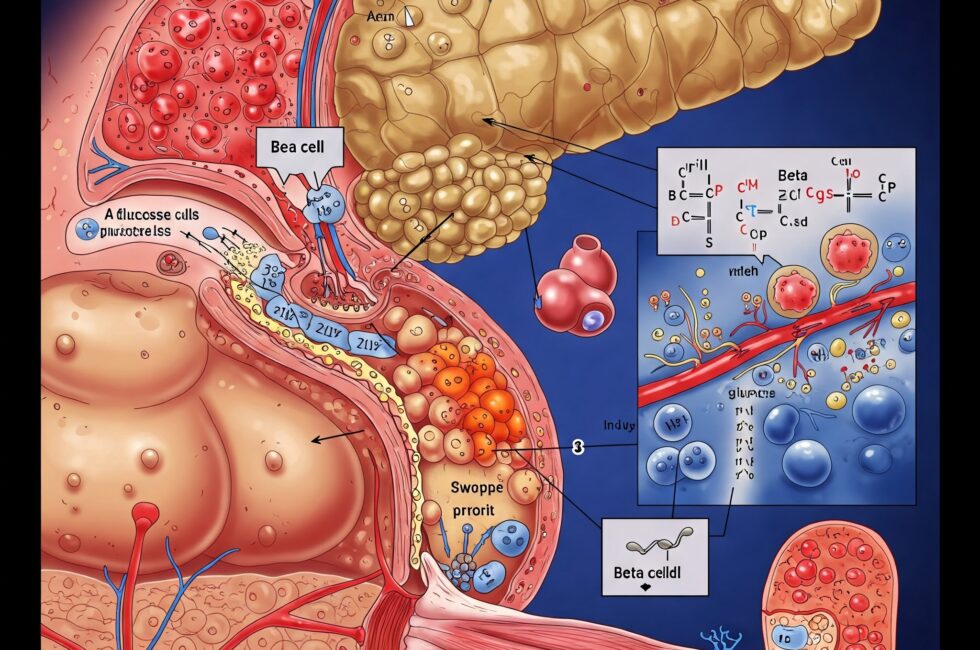
At its core, insulin resistance is a condition where cells in the body become less responsive to insulin, the hormone responsible for facilitating glucose uptake from the bloodstream. According to Dr. Bikman, insulin resistance has two inseparable facets: reduced insulin signaling and hyperinsulinemia. The first aspect refers to certain cells—such as those in muscle, liver, or fat tissue—not responding efficiently to insulin’s signal to take up glucose. This is not a universal phenomenon but is tissue-specific, meaning some cells may remain insulin-sensitive while others become resistant.
The second facet, hyperinsulinemia, is characterized by elevated insulin levels in the blood. Bikman emphasizes that hyperinsulinemia often precedes reduced insulin signaling and is a hallmark of insulin resistance. “There is no such thing as insulin resistance without there being an accompanying and often preceding hyperinsulinemia,” he states. This elevation in insulin levels is the body’s attempt to compensate for reduced cellular sensitivity, maintaining normal blood glucose levels despite the underlying dysfunction.
Understanding both aspects is critical because focusing solely on blood glucose, as is common in conventional medical practice, can mask the early stages of insulin resistance. Glucose levels may remain normal for years or even decades while insulin levels climb, silently contributing to metabolic dysfunction. This glucose-centric paradigm, Bikman argues, misses the root cause: disordered insulin action.
The Chronological Progression of Insulin Resistance
Insulin resistance is not an overnight phenomenon; it develops gradually, often over decades, with distinct stages that impact various tissues in the body. Bikman outlines this progression as follows:
Early Stages: Silent Dysfunction
In the initial stages, insulin resistance begins with certain cells—often fat cells—becoming less responsive to insulin. To compensate, the pancreas produces more insulin, leading to hyperinsulinemia. This phase can persist for years without noticeable symptoms, as glucose levels remain within an acceptable range. However, other health issues may emerge, such as weight gain, hypertension, infertility, or migraines, which are often linked to underlying insulin resistance but not recognized as such due to the medical focus on glucose.
Tissue-Specific Progression
As insulin resistance progresses, it affects additional tissues beyond fat cells. The liver, a key regulator of glucose production, becomes insulin-resistant, disrupting processes like glycogenesis (glycogen formation), glycogenolysis (glycogen breakdown), and gluconeogenesis (glucose synthesis from non-carbohydrate sources). This dysregulation contributes to impaired glucose management.
Muscle tissue, which normally accounts for a significant portion of glucose uptake, also becomes insulin-resistant, reducing its glucose uptake capacity by about 50%. The alpha cells in the pancreas, responsible for glucagon production, are similarly affected, further complicating blood sugar regulation. These changes mark a critical shift, as the body’s ability to maintain normal glucose levels begins to falter.
Clinical Detection: The Glucose Spike
Insulin resistance typically becomes clinically detectable only when glucose levels start to rise, often years after the onset of hyperinsulinemia. At this point, the body may struggle to produce enough insulin to compensate for the resistance, though Bikman notes that insulin levels rarely drop to zero in type 2 diabetes. Instead, they remain elevated compared to pre-disease levels, contributing to a host of metabolic issues.
When glucose levels climb, the medical focus shifts to managing blood sugar, often through insulin therapy or glucose-lowering medications. However, Bikman warns that this approach can exacerbate the problem. “Giving a type 2 diabetic insulin is like giving an alcoholic another glass of wine hoping it will cure their alcoholism,” he quips. High insulin doses can lead to weight gain, a lower metabolic rate, and increased insulin resistance, creating a vicious cycle. Alarmingly, type 2 diabetics requiring more insulin to control glucose are three times more likely to die from heart disease, highlighting the dangers of this approach.
Physiological vs. Pathological Insulin Resistance
Not all insulin resistance is harmful. Bikman distinguishes between physiological insulin resistance, which serves a beneficial purpose, and pathological insulin resistance, which drives chronic disease.
Physiological Insulin Resistance
Physiological insulin resistance occurs naturally during specific life stages, such as pregnancy and puberty, to support growth and development. During pregnancy, insulin resistance allows glucose to be prioritized for the fetus, while hyperinsulinemia supports maternal fat accumulation. “You don’t want to mitigate it…it would be utterly incompatible with the pregnancy,” Bikman explains. Similarly, during puberty, insulin levels can double to promote growth, particularly in insulin-sensitive tissues like bone.
In both cases, insulin resistance is tissue-specific, allowing certain cells to remain responsive while others become temporarily resistant. This controlled resistance is essential for meeting the body’s increased metabolic demands. Bikman also debunks the myth that low-carb or ketogenic diets cause physiological insulin resistance, clarifying that such diets do not mimic these natural states.
Pathological Insulin Resistance
In contrast, pathological insulin resistance is a chronic, harmful state that contributes to metabolic disorders. It is driven by factors like poor diet, sedentary lifestyle, and genetic predisposition, leading to widespread cellular dysfunction. Unlike physiological insulin resistance, which is temporary and purposeful, pathological insulin resistance persists, causing long-term damage to tissues and increasing the risk of conditions like type 2 diabetes, heart disease, and hypertension.
Adipose Insulin Resistance (Adipo-IR): An Early Warning Sign of Chronic Disease
One of Bikman’s key contributions is his focus on adipose insulin resistance (Adipo-IR), which he believes is among the earliest markers of metabolic dysfunction. Fat tissue is often the first to become insulin-resistant, making Adipo-IR a critical indicator.
The Adipo-IR index measures insulin resistance in fat cells by assessing fasting insulin and free fatty acid levels. In healthy individuals, high insulin levels suppress lipolysis (fat breakdown), keeping free fatty acids low. In insulin-resistant individuals, however, fat cells continue to release free fatty acids despite elevated insulin, leading to high levels of both. This dysregulation reflects a breakdown in insulin’s ability to regulate fat metabolism, providing an early clue to metabolic issues.
Adipo-IR is particularly relevant because it can detect insulin resistance in individuals who may not yet show classic symptoms, such as those with polycystic ovary syndrome (PCOS). By identifying dysfunction early, interventions can be implemented to prevent progression to more severe metabolic disorders.
Insulin, Triglycerides, and Heart Disease
Bikman challenges the conventional focus on LDL cholesterol as the primary predictor of heart disease, arguing that triglycerides are a far better indicator. Insulin plays a central role in triglyceride synthesis, or lipogenesis, in the liver. When insulin levels are high, the liver produces more triglycerides, which are packaged into lipoproteins like VLDL and LDL. Elevated triglycerides, rather than LDL, are strongly correlated with heart disease risk.
Carbohydrate restriction can dramatically lower triglyceride levels, as it reduces insulin production. Bikman notes that triglycerides respond quickly to dietary changes, making them a dynamic marker of metabolic health. In contrast, LDL levels may rise on low-carb diets, but if accompanied by low triglycerides and high HDL, this profile is associated with longevity. “Congratulations, you’re probably going to live longer,” Bikman says of such individuals.
The lack of pharmaceutical options for lowering triglycerides, compared to the abundance of LDL-lowering drugs, may explain the clinical bias toward LDL. However, Bikman advocates for a shift in focus to triglycerides and insulin management to better address cardiovascular risk.
Insulin and mTOR: Implications for Longevity
The mTOR pathway, which regulates cell growth and proliferation, is another area where insulin plays a significant role. While dietary protein can activate mTOR, Bikman emphasizes that insulin is a far more potent stimulator. Chronically elevated insulin, common in insulin-resistant individuals, leads to prolonged mTOR activation, which may accelerate aging and reduce longevity.
For those aiming to moderate mTOR activity, controlling insulin levels is more effective than restricting protein intake. This is particularly relevant given insulin’s prolonged elevation after consuming starches and sugars, compared to the transient rise in amino acids from protein. By prioritizing low-insulin dietary strategies, individuals can optimize mTOR signaling for health and longevity.
Dietary Strategies for Managing Insulin Resistance
Bikman’s dietary recommendations center on lowering insulin levels to address the root cause of insulin resistance. Key principles include:
- Protein Quality: Animal-based proteins are superior due to their complete amino acid profile, which supports muscle protein synthesis and overall health. Plant-based proteins, while viable, should be fermented to improve absorption and reduce anti-nutrients like oxalates and phytic acid. Bikman stresses that protein should always be consumed with fat, as bile acids facilitate digestion. “In nature, there is no such thing as a protein that does not come with fat,” he notes.
- Optimal Fats: Fats from animal sources and fruits like avocados, coconuts, and olives are considered “ancestral” and beneficial. These fats support metabolic health and do not contribute to insulin resistance. While chicken is acceptable, other meats are nutritionally superior due to their higher fat content.
- Low-Insulin Strategies: A low-insulin approach prioritizes protein, embraces healthy fats, and limits carbohydrates, particularly refined starches and sugars. This contrasts with low-energy (calorie-restricted) diets, which can lead to hunger and fail to address insulin resistance. By reducing insulin, the body can access fat stores more effectively, promoting fat loss and metabolic health.
- Ketogenic Advantage: Ketogenic diets, which induce ketogenesis (ketone production), offer a metabolic advantage by increasing energy expenditure. Ketones are excreted in breath and urine, effectively “wasting” calories, and studies suggest a ketogenic state can boost metabolic rate by up to 300 calories per day. This fat-burning state aligns with Bikman’s emphasis on low-insulin strategies.
- Time-Restricted Feeding: Eating earlier in the day aligns with the body’s circadian rhythms, optimizing metabolic health. Bikman advises consuming more calories during the day and less at night to support sleep quality and metabolic function.
Conclusion: A Paradigm Shift in Metabolic Health
Dr. Ben Bikman’s insights into insulin resistance challenge the glucose-centric paradigm that dominates conventional medicine. By highlighting the dual nature of insulin resistance—reduced signaling and hyperinsulinemia—he underscores the importance of measuring insulin levels to detect metabolic dysfunction early. His focus on adipose insulin resistance, triglycerides, and low-insulin dietary strategies offers a roadmap for preventing and managing insulin-related disorders.
Insulin resistance is not just a precursor to type 2 diabetes; it is a fundamental driver of chronic conditions like heart disease, hypertension, and infertility. By addressing the root cause—elevated insulin—through targeted dietary and lifestyle interventions, individuals can reclaim their metabolic health. As Bikman aptly summarizes, “The glucose levels are themselves simply a symptom or a manifestation of disordered insulin action.” The link between insulin and chronic disease provides a foundational understanding for embracing a holistic health approach.